Experts Call for Individualized, Evidence-Based Cancer Pain Treatment Model
The biopsychosocial approach to individualizing
assessment and treatment of cancer pain should become the mainstream
approach and a new model is needed to make it even more widely
accessible and implemented.
That was the bottom line of a presentation by a Dutch cancer pain
professor at the 7th World Congress of the World Institute of Pain
(WIP), held recently in Maastricht, Netherlands; it was also the opinion
of pain experts on this side of the Atlantic, who are developing
guidelines to reflect the modern understanding of cancer pain
management.
The three-step model for pain medicine published by the World Health
Organization (WHO) in 1986 for the management of cancer pain (http://www.who.int/cancer/palliative/painladder/en/)
is still being used but does not allow for individualized diagnosis and
treatment, said Kris C.P. Vissers, MD, PhD, president-elect of the WIP
and research chair, Department of Anesthesiology, Pain and Palliative
Medicine, Radboud University Medical Center, Nijmegen, Holland. In
contrast, the biopsychosocial approach takes into account the
psychological state of the patient, the patient’s social support and his
or her values and sense of spirituality, he said. It also emphasizes a
thorough assessment of the causes of the pain.
This holistic view of pain is able to account for the significant
variations in the amount of pain, suffering and resulting coping
behaviors among patients with the same anatomical abnormalities, or lack
thereof, Dr. Vissers said.
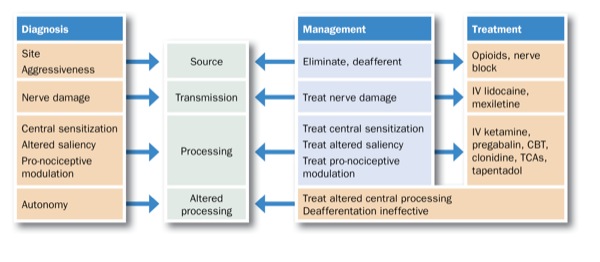
He proposed that physicians use a four-pronged framework for
assessing and diagnosing each patient with cancer pain. These focus on
the pain source/site; how that pain is propagated and processed; and
whether the pain processing is altered in some way at some point in the
body (see Figure).
“We have the knowledge to be able to do provide these ‘medical
reasoning models’ routinely in clinical practice every day with every
pain patient but we’re not implementing them. If a primary care provider
refers a patient then he should provide a medical hypothesis for that
patient’s pain, including the site, the nerve damage and whether there
is central desensitization,” Dr. Vissers said. “This information is
necessary to provide the correct therapy, rather than just providing
broad, empiric therapy.”
He believes that quantitative sensory testing should be used to
determine the magnitude of sensory abnormalities in pain patients. He
also proposed the use of centralized databases to collect information on
validation of assessment tools, patient diagnoses, treatments and
long-term outcomes. This will lead to continuous improvement and
standardization in use of assessment tools, increased accuracy, reduced
cost of diagnosis and treatment, and improved education and training of
health care professionals who treat pain patients.
Two American pain experts contacted by Pain Medicine News
agreed it is important to supplant the outdated WHO pain treatment
algorithm with a more nuanced, evidence-based and individualized
approach, and to make sure it is implemented in a standard way.
“The biopsychosocial model Dr. Vissers described and variations of it
have been implemented in various cancer institutions including ours,”
said Amitabh Gulati, MD, director of ambulatory pain, Department of
Anesthesia and Critical Care, Memorial Sloan-Kettering Cancer Center,
New York City. “Our palliative, psychiatry, rehabilitation and
anesthesiology services meet regularly to discuss patients who have
complex pain symptoms and develop a comprehensive plan similar to that
described by Dr. Vissers.”
Brian Bruel, MD, an assistant professor of pain medicine, University
of Texas MD Anderson Cancer Center, Houston, and president-elect of the
Cancer Pain Research Consortium, said his group was formed last year to
develop guidelines that “fill the holes” in the care of cancer patients
with pain. He added that Dr. Gulati is also a member of the consortium.
“Dr. Vissers brought up some very good points; he showed that there
are some gaps in our management of cancer pain,” he said. “Our
consortium is approaching this in a parallel way. In June 2014, we held a
multi-institutional and multidisciplinary meeting involving
neurosurgery, anesthesia, physical medicine and rehabilitation,
psychology, and medical and radiation oncology, in order to come up with
discipline-specific best practices. That’s an important step toward
creating new evidence-based guidelines for pain management in cancer
patients.”
—Rosemary Frei, MSc
No comments:
Post a Comment